|
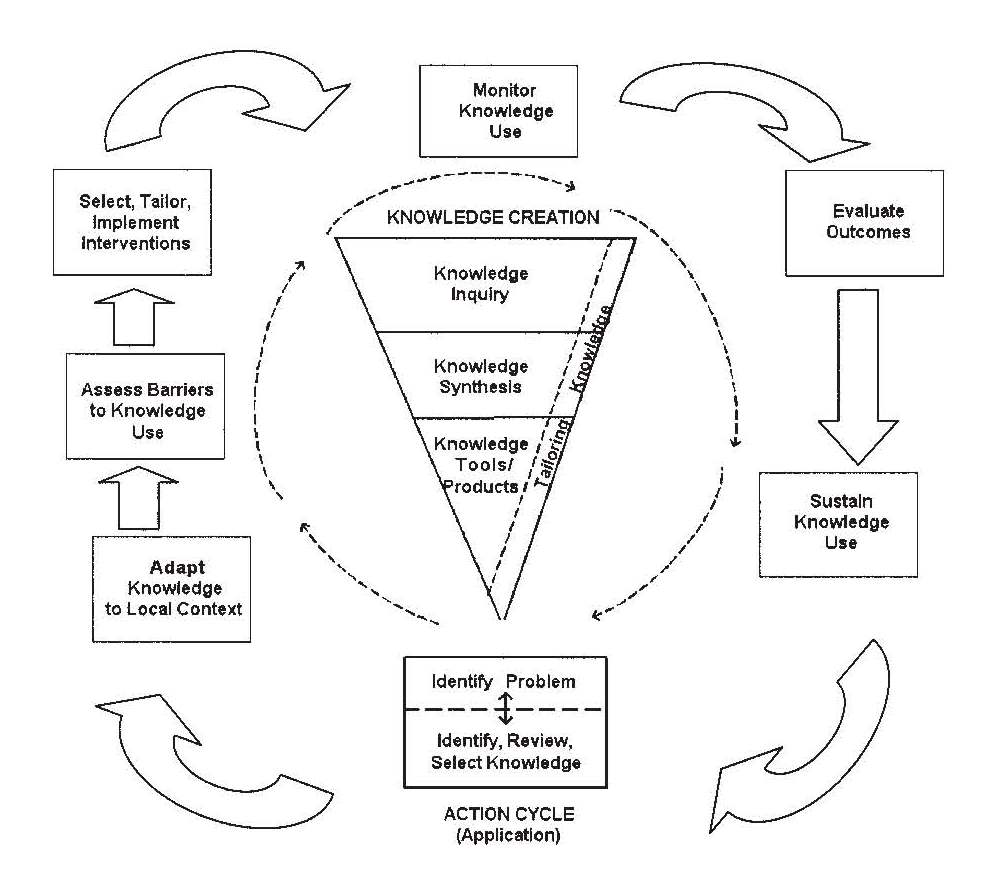
Knowledge creation. Within the KTA framework, knowledge creation is depicted as a funnel whereby knowledge is repeatedly refined and synthesized, ultimately leading to knowledge tools and/or products. The first stage, knowledge inquiry, refers to the continually growing knowledge base in, for example, pediatric pain. In the KTA model, knowledge inquiries are further refined through synthesized packages (e.g. systematic reviews). Finally, the funnel of knowledge creation ends with a concrete tool or product (e.g. practice guidelines) designed for use by key stakeholders of that knowledge (e.g. clinicians, policy makers).
While the focus in knowledge translation is naturally on dissemination, additional attention should be paid to the knowledge creation phase of the KTA process model. One important issue to address at this stage is the development of methodologically sound research that also considers the clinical setting (Kazdin & Kendall, 1998). Foundational studies of pediatric pain may not necessarily translate into clinically relevant results. While this type of intervention research is still extremely important to developing work in pediatric psychology (Blount, 1987), the emphasis needs to shift towards creating clinically meaningful interventions. Additionally, original investigations often do not consider the pragmatic factors associated with the implementation of psychologically-based interventions in the real world. Factors worthy of consideration in this type of research include the intervention’s utility, the time required for training and implementation, as well as health professionals’ satisfaction with and preference among various available strategies (Blount et al., 1999). Finally, additional efforts need to focus not only on advocating for the use of psychological interventions, but also on creating interventions attractive to those in charge of making and implementing health care policies. As health care and insurance systems continue to attend to and support more invasive pain management strategies (Craig et al., 1996), psychological researchers need to be more prepared to advocate for their own non-invasive approaches. In the end, factors such as the cost-effectiveness of many psychological interventions may be of the utmost importance as constraints on the healthcare budget increase (Drotar, 1997).
Knowledge application. The knowledge application portion of the model is depicted as a cycle highlighting the recurring nature of knowledge translation. The starting point of the process is identifying a target problem and reviewing existing literature for the solution. Once identified, the knowledge is modified and refined to reflect the needs and constraints of the context in which it will be implemented. Next, barriers to knowledge use are explicitly identified, followed by selecting and tailoring the chosen intervention. Upon implementation, the final stages include monitoring the use of the translated knowledge, evaluating targeted outcomes (e.g. pain intensity) and finally, implementing strategies to sustain knowledge use over time.
While knowledge translation is the term most commonly used (Graham et al., 2006), it is often critiqued for suggesting a unidirectional process in which knowledge is simply translated to the targeted population. The KTA process model, on the other hand, focuses on action (not translation) and aims to include feedback and suggestions from all necessary stakeholders at every step in the process. For pediatric pain, the relative simplicity of many psychological interventions (e.g. distraction) has facilitated the incorporation of multiple stakeholders in delivering appropriate pain management. In fact, many encouraging attempts have already been made to train health professionals (Lasch et al., 2000), paramedical professionals (Solomon et al., 1998) and parents (Manimala et al., 2000) to use these strategies to reduce and manage pediatric pain. However, additional efforts need to be focused on increasing the long-term success of these translation efforts (MacLaren & Cohen, 2005). Increased training in and exposure to psychological pediatric pain interventions provide not only the opportunity to increase knowledge about psychological pain management, but also to increase health professionals’ motivation to change their own clinical practices (Craig et al., 1996). Involving hospital administration further serves to support these endeavors. Moreover, with the ever-increasing acceptance of psychological pain management strategies, the environment of healthcare is now optimal for incorporating multiple disciplines to manage pediatric pain. In the cost-conscious world of healthcare, the possible reduction of cost when incorporating non-pharmacological approaches (e.g. Cohen et al., 1999) and the ability to further reduce costs by incorporating multiple health professions in a medical setting (Powers, 1999) becomes increasingly important.
Broader issues
While beyond the scope of the current commentary, factors beyond the KTA model are also important to consider in improving knowledge translation efforts. Researchers are not typically trained in the art of policymaking; thus, increased exposure to this important aspect of knowledge translation should be included in the training of future researchers. Additionally, funding bodies, and even research ethics boards, have begun and will continue to press for researchers to explicitly state the populations for which their results are intended. Considering this issue in the design phase of research may help to ensure the resulting knowledge is successfully translated to the target population. These broader issues will require additional focus and clarity over time, as knowledge translation efforts come to the center of attention.
Conclusion
Psychological interventions, though established as effective in managing pediatric pain, have not been successfully translated into everyday clinical practice. The problem of effective dissemination, as well as the lack of clinically meaningful research, creates a large gap between the care that could be given and the care that is being received by pediatric patients experiencing pain. While organizations such as the American Pain Society are attempting to provide large-scale, macro-level solutions to this problem (Ness et al., 2007), additional efforts at the level of the individual researcher are needed to supplement this work. As highlighted in the KTA process model, projects aimed at knowledge translation should continue to work towards developing better methods to create and translate effective interventions. In fact, though not exclusively focused on psychological interventions, many projects are currently underway using theory-driven translation efforts (e.g. the Canadian Institutes of Health Research [CIHR] funded Team in Children’s Pain, www.childrenspainstudy.ca). It is only through the development of clinically relevant interventions, continued advocacy and policy reform, effective dissemination, and incorporation of multiple health professions that children will be given the greatest access to the pain management strategies the field of pediatric psychology has spent so many years carefully developing.
Acknowledgment
The author would like to thank Christine Chambers, Carl von Baeyer, and three anonymous reviewers for their editorial comments and suggestions on earlier versions of this commentary. N.F. Bandstra is supported by an IWK Health Centre Graduate Student Research Scholarship and an honorary Killam Predoctoral Scholarship. She is a trainee member of Pain in Child Health, a Strategic Training Initiative in Health Research of CIHR.
Nancy F. Bandstra, BSc (Hons)
Doctoral Student,
Department of Psychology, Dalhousie University and
Centre for Pediatric Pain Research, IWK Health Centre, Halifax, Nova Scotia, Canada
email: nancy.bandstra [at] dal.ca |
References
Blount RL. The dissemination of cost-effective psychosocial programs for children in health care settings. Child Health Care 1987;15:206-213.
Blount RL, Schaen ER, Cohen LL. Commentary: current status and future directions in acute pediatric pain assessment and treatment. J Pediatr Psychol 1999;24:150-152.
Cohen LL, Blount RL, Cohen RJ, Schaen ER, Zaff JF. Comparative study of distraction versus topical anesthesia for pediatric pain management during immunizations. Health Psychol 1999;18:591-598.PubMed Abstract
Craig KD, Lilley CM, Gilbert CA. Social barriers to optimal pain management in infants and children. Clin J Pain 1996;12:232-242. PubMed Abstract
Cummings EA, Reid GJ, Finley GA, McGrath PJ, Ritchie JA. Prevalence and source of pain in pediatric inpatients. Pain 1996; 68:25-31. PubMed Abstract
Dahlquist LM, Switkin MC. Chronic and recurrent pain. In: Roberts MC, editor. Handbook of pediatric psychology, third edition. New York: Guilford, 2003. pp. 198-215.
Drotar D. Intervention research: pushing back the frontiers of pediatric psychology. J Pediatr Psychol 1997;22:593-606. PubMed Abstract
Ellis JA, O’Connor BV, Cappelli M, Goodman JT, Blouin R, Reid CW. Pain in hospitalized pediatric patients: how are we doing? Clin J Pain 2002;18:262-269. PubMed Abstract
Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, Robinson N. Lost in translation: time for a map? J Contin Educ Health Prof 2006;26:13-24. PubMed Abstract
Kazdin AE, Kendall PC. Current progress and future plans for developing effective treatments: comments and perspectives. J Clin Child Psychol 1998;27:217-226. PubMed Abstract
Lasch KE, Wilkes G, Lee J, Blanchard R. Is hands-on experience more effective than didactic workshops in postgraduate cancer pain education? J Cancer Educ 2000;15:218-222. PubMed Abstract
MacLaren JE, Cohen LL. Teaching behavioral pain management to healthcare professionals: a systematic review of research in training programs. J Pain 2005;6:481-492. PubMed Abstract
Manimala MR, Blount RL, Cohen LL. The effects of parental reassurance versus distraction on child distress and coping during immunizations. Child Health Care 2000;29:161-177.
McMurtry CM, McGrath PJ, Chambers CT. Reassurance can hurt: Parental behavior and painful medical procedures. J Pediatr 2006;148:60-61.
Ness T, Wesselmann U, Stone L, Mantyh P, Neubert J. The American Pain Society and translational pain research: a position statement from the American Pain Society. March 21, 2007. www.ampainsoc.org/advocacy/downloads/translationalpain.pdf
O’Byrne KK, Peterson L, Saldana L. Survey of pediatric hospitals’ preparation programs: evidence of the impact of health psychology research. Health Psychol 1997;16:147-154. PubMed Abstract
Powers SW. Empirically supported treatments in pediatric psychology: procedure-related pain. J Pediatr Psychol 1999;24:131-145. PubMed Abstract
Solomon R, Walco GA, Robinson MR, Dampier CD. Pediatric pain management: program description and preliminary evaluation results of a professional course. J Dev Behav Pediatr 1998;19:193-195.
Uman LS, Chambers CT, McGrath PJ, Kisely S. Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev 2006 Oct 18;4:CD005179. PubMed Abstract
|